Eating Disorder Resources for Families
We believe in our patients' capacity to fully recover and build resiliency. In addition, we know that family & friend involvement in the treatment and recovery journey is invaluable. Our goal is to equip you to support your loved ones through a variety of educational resources:
- Learn about the unique causes, research, medical complications, and treatment of eating disorders
- Gain valuable information on how to best support a loved one with an eating disorder
- Feel more confident as a proactive, knowledgeable support person in your loved one’s recovery journey
- Become connected with your loved one’s ERC treatment team and clinicians

Helping a Loved One Recover from an Eating Disorder
Emotion-Focused Family Therapy with Elizabeth Easton, Psy.D
Dr. Easton is the Regional Director of Child & Adolescent services. Dr. Easton’s four-part presentation is designed for families to learn about their role in recovery and the skills to become recovery coaches. If you have every wondered “how can I help my loved one recover from an eating disorder?” this is the video training series for you. The skills taught here apply to “caregivers” meaning anyone who is providing care to a patient in treatment, no matter the age of the patient or the age of the caregiver. Learn how to harness your caregiver power.
Welcome
Emotion Basics
Step 1
Step 2
Anger
Silence/Shut Down
Eating Disorder Recovery Books
Hope Orientation for Family & Friends

All the various stages of treatment are important, but the beginning is a critical foundation to them all. Our free, Hope Orientation for Family and Friends helps you establish a strong beginning, middle, and end of your time with us. We’ll guide you through next steps, practical tips for how to make the most of treatment, and best ways to support your loved one during their early stages of recovery.
During this orientation, learn about:
- What benefits each level of care offers and how they tie together
- Who your loved one’s treatment team is and when you’ll connect with them
- When you can be involved and why your participation is important
- How to prepare for the end of treatment and when to start getting ready
We know the process of trusting us and continuing to support your loved one through these next steps is no small task. While there are often many questions about the unknown, we’re here to help answer them – and navigate this journey with you.
Takes place every Wednesday at 11:00 am MT.
The Hope Orientation includes a presentation via Zoom, followed by Q&A.
Coming together each week with other families, friends and support systems who can relate and empathize with your experience helps you form a community of personal bonds and connections.
Eating Disorder Support Groups for Families
Eating Recovery Center offers free, trained facilitator-led, support groups for those struggling with eating disorders (including anorexia, bulimia, binge eating disorder and other disordered eating issues). ERC additionally provides support groups for families and community members to deliver resources and education on eating disorder treatment and recovery.


Stay Connected with Your Recovery Community
Are you or a loved one on the path to recovery? Our new opt-in form enables you to stay connected with our team and continue to receive support after discharge and throughout your or a loved one's recovery journey. By signing up, you'll receive the latest free resources, including access to support groups, upcoming events, educational materials, and more.
Virtual Family & Friends Education Series

Stay the Course: Practical Steps to Support
Your loved one has moved through higher level of care (HLOC), and they are transitioning back to life outside of treatment. As a caregiver, you play a vital role in helping your loved one move through recovery. We want to make sure you have the practical tools to help everyone carry on. Join us for the Stay the Course: Practical Steps to Support presentation to help identify ways that you can offer ongoing help and encouragement. This presentation will prepare you for the aftercare and wellness planning process.

Events
We are proud to offer a variety of events and educational opportunities to our alumni, families, caregivers, professionals and community members.


Beth Ayn Standfield, M.Ed.
National Family Advocate
Eating Disorders 101
2nd Saturday of each month | 10:00 - 11:00 am ET | 1 CE Credit
This presentation includes a look at the contributing factors and maintenance factors of eating disorders, an overview of the commonly referenced eating disorders and access to online screening tools to help with early detection and treatment. With lived experience, anecdotes and an abundance of resources, attendees are guaranteed a unique, practical experience. Q & A portion follows the talk.
Eating Disorders 201
4th Saturday of each month | 10:00 - 11:00 am ET | 1 CE Credit
This presentation includes a review of what treatment looks like for those diagnosed with an eating disorder and how recovery impacts their life. With this focus, a great amount of time will be spent on discussing practical tools and ways in which to offer emotional and practical support in the school, the college and the work setting. With lived experience, anecdotes and an abundance of resources attendees are guaranteed a unique, practical experience. Q & A portion follows the talk.
Consider Eating Disorders 101 for School Professionals, Community Members and Caregivers prior to attending.
What to Expect in Eating Disorder Treatment
In addition to experiencing some hesitation around treatment, your loved one will acclimate to a new setting, people, and expectations. Treatment is challenging and can often feel uncomfortable.
Medical and psychiatric stability need to be obtained before your loved one has the cognitive and physical resources to fully work on insight-oriented psychotherapy. Nutritional rehabilitation begins on the first day of treatment and is foundational to both mental and medical treatments. As medical and psychiatric stability are achieved, your loved one will be able to more deeply engage in the psychoeducation and skill-development necessary to achieve behavioral change.

Getting matched with the exact support they need.
With one conversation, our mental health professionals will help your loved one better understand what they’re going through and what they need.
We will meet them where you are, listen to their story in a therapeutic setting, and match them with the level of support that meets their struggle.
Travel Accommodations
Choosing where you seek treatment for an eating disorder or mood and anxiety disorder is a big decision, including where your center of choice is located. Many times the best choice for you will not be in your area.
Patients and their families travel from all 50 states across the U.S. and from every continent throughout the world to our treatment centers so that they can receive the best possible treatment. We are honored that families travel from near and far to be with us. We also recognize how stressful and overwhelming it is to make travel arrangements while you’re making that next big step towards treatment.
Treatment Modalities
Eating Recovery Center offers supportive, compassionate treatment for eating disorders provided by renowned experts in the field. With an emphasis on sustained recovery following treatment, our multidisciplinary teams offer comprehensive, individualized treatment plans focused on an evidence-based approach to healing. Therapeutic approaches include Acceptance and Commitment Therapy (ACT), Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), Radically Open DBT, and Exposure and Response Therapy.
Frequently Asked Questions
-
Should family members stay nearby when a loved one is in eating disorder treatment?
While your loved one is in our care, we frequently suggest that family members and friends return home to care for themselves and other family members, and rest and restore. We also understand that every individual is different and personal circumstances often vary.
Please communicate with the ERC treatment team if you feel that you should stay near your loved one’s treatment center. We will work with you to help make the decision and arrangements that are best-suited for your family.
-
Where can I find eating disorder support for families and caregivers?
As a caregiver, you may feel incredibly overwhelmed and overloaded. Know that it is normal to feel this way, particularly as you take a big step into the unknown with your loved one.
You are not alone! Our entire team of Community Outreach Liaisons, National Family Outreach Manager, and National Family Advocate are all available to answer questions or lend a listening ear. Contact us at [email protected].
-
What is the typical length of eating disorder treatment?
You may wonder how long your loved one will be in our care. While the treatment journey is different for each person, key markers of recovery include Mental/Emotional Stability, Medical Stability, and Insurance Coverage.
-
What are the key markers of recovery?
All distressing and harmful behaviors – and any serious or acute mood disturbances – will need to be understood, addressed, and treated. Behaviors including starvation, purging, binging, excessive exercise, substance use, and self-harm have been used to help your loved one avoid difficult feelings and thoughts. Yet these behaviors that once served to help them cope ultimately become serious problems.
-
What can I expect in terms of insurance and payment?
Insurance companies will sometimes have different criteria and standards for how long your loved one can remain in treatment. While we work closely with third party payers, ultimately – if you are using insurance for treatment – they have the final say regarding length of stay.
More often than not, we are in full agreement with insurance providers regarding treatment plans and length of stay. If a situation arises and we are not aligned, our dedicated business office staff will help you advocate with insurance providers and answer any questions.
-
Will I be able to communicate with my loved one? Will I be able to contact their care team?
Yes, you can communicate with your loved one. Your loved one will have access to their electronics throughout the treatment day. Yes, you can communicate with the care team. C&A family members will be contacted by the care team the day of admission and will be included in all stages of treatment. Family members of adult patients are invited and encouraged to be a part of the treatment process. Adult patients must complete paperwork giving the care team consent to communicate with family members.
-
How frequently can I visit my loved one while in treatment? At what point is visitation allowed?
Family and friends are welcome to visit their loved ones in treatment. Please contact the care team to discuss what is supportive for the patient. The care team can provide details re: the specific visitation information.
-
Am I permitted to send mail and/or packages to my loved one?
Yes, mail and packages are welcomed. Please talk with the care team to learn more about the mailing address.
-
How will I know when we are nearing a discharge date?Planning for discharge will be discussed with you, the care team and the patient. It is important to plan for a seamless step down by completing IOP and scheduling outpatient appointments before discharging.
Typical First Week
For patients at a higher level of care, your loved one will arrive for the first day of treatment in the morning. Within the first week, your loved one will be introduced to a number of key treatment team members, including:
- A nurse for a physical assessment and labs
- A doctor for a medical assessment and review of any complications, issues, or specific needs
- Your treatment team (psychiatrist, therapist, and registered dietitian) A business office representative who will discuss insurance benefits, payment, and other logistical details
- A staff member who will help your loved one become familiar with the treatment center and settle into the space
Most patients have a similar schedule for their first week of treatment, although individual experiences do vary by program and level of care.
Moving Forward in Recovery
The entire treatment process may seem extremely challenging, and difficult to understand. Our overarching purpose is to help your loved one:
- Establish a normalized eating pattern and routine
- Feel comfortable eating in social situations
- Eat appropriate and adequate nourishment
- Disrupt eating disorder behaviors
Moreover, our programming focuses on helping your loved one replace unhealthy coping mechanisms with healthy coping Strategies.
Dealing with Challenges
Physical and emotional challenges can occur when your loved one begins to adopt healthier eating behaviors. The structured, supportive environment of treatment will help your loved one’s recovery:
- If your loved one has been significantly restricting food, we will work on gradually increasing intake at a safe, steady rate while monitoring lab values and fluid balance.
- To minimize discomfort (stomach pain, constipation, etc.) as the digestive system adapts to regular eating, the dietitian will work closely with the medical team and monitor the meal plan volume and contents.
Support is a key component in learning healthy coping skills to help manage the anxiety that arises when reintroducing foods and increasing variety.
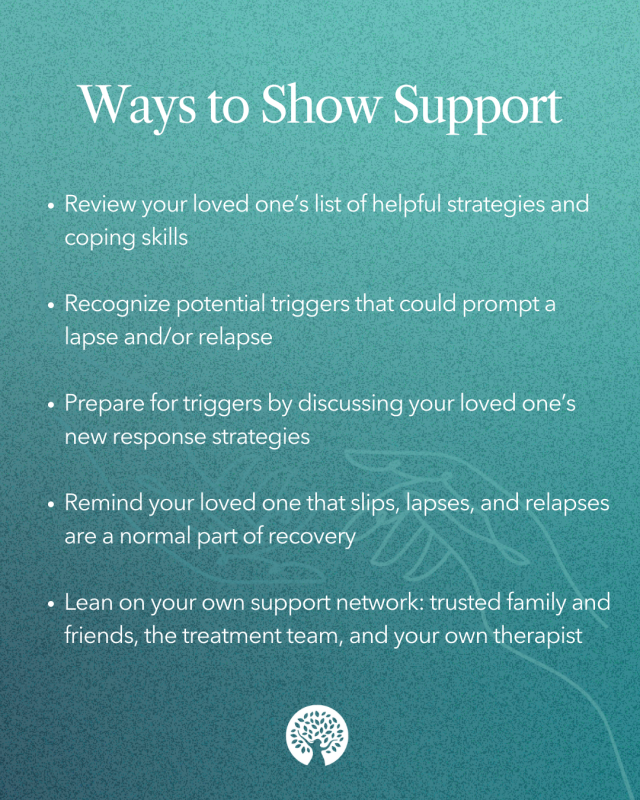
Eating Disorder Relapse Prevention
Patients are involved in what we call relapse prevention programming: thinking through and making plans on how to address the challenges of recovery in their home environment. At ERC, we also call these wellness plans, or relapse reliance plans. Patients will begin to actively work on their plan as they near the end of treatment.
Keep in mind that your loved one will discharge from treatment into a “hostile recovery environment.” Our Western society continues to stigmatize mental health disorders and care. Additionally, we live in a culture of “do more, get more, be more” which can drive and reinforce perfectionism. The fast pace and cultural expectations can make it very challenging for our loved ones to prioritize the processes and tasks of recovery once they return home, as doing so requires they act and behave differently than their peers and social groups.
While the recovery process will have ups and downs, some successes and some stumbles, it is important to hold hope that treatment will instill your loved one with increased awareness and recovery skills.

Eating Disorder Treatment Programs
ERC offers programming and services to support your loved one’s health and protect recovery at every level of care in eating disorder treatment. At ERC, your loved one will work with a team of compassionate, highly trained clinicians who will collaborate on an individualized treatment plan that emphasizes building skills, confidence, and support to maintain recovery after treatment.
At each level of care, our evidence-based treatment approach utilizes behavioral interventions that not only address symptoms, but also seek to understand the underlying meaning and function of behaviors.

Levels of Care
Treatment Team
Throughout treatment, your loved one will be surrounded by a team of experts who specialize in eating disorders and other co-occurring mental health conditions. The same team will work closely and collaboratively on all aspects of your loved one’s care.
Your loved one may already have an established treatment team, or a close outpatient provider. Our goal is to work in partnership with other specialists and treatment team members to help achieve the best possible chance for recovery.

Treatment Sessions
The specific goals of family and caregivers will depend on the information gathered during the pre-admission assessment process: used to develop your loved one’s individualized treatment plan.
A variety of sessions are a critical component of your loved one’s programming during treatment, with sessions generally held each week. You can expect to learn more during admission, at which point the treatment team will discuss all aspects of your loved one’s treatment.

-
Individual Sessions
Each week, patients have scheduled sessions with their primary therapist. The primary therapist may also interact with your loved one in group or meal support settings. Individual psychotherapy focuses on helping your loved ones identify what is important to their lives, and learn the necessary skills to keep their dedication and focus on these things.
-
Group Therapy
Groups offer patients the opportunity for insight, validation, and support from peers who understand and have experienced similar challenges. Group therapy is where your loved one will develop new perspectives and insights, while learning skills and strategies for coping with life’s challenges. Your loved one’s schedule will include two to four groups each day.
-
Nutritional Rehabilitation
The interruption of eating disorder behaviors, normalization of eating processes, and weight restoration are the focus of our nutrition rehabilitation process. Education surrounding nutrition, meal planning, and weight normalization and restoration are target goals.
-
Family Therapy
The goal for families, caregivers, and support persons is to provide a place of understanding, compassion, and non-judgement. Family therapy will focus on education and skill-building, as participants learn advanced caregiver skills and are guided to apply their new skills as they support loved ones.
Family involvement is especially critical for the parents of younger patients in child & adolescent programming. The treatment approach for patients ages 8 through 17 is rooted in Family-Based Treatment (FBT), which empowers parents to become agents of change in the recovery of their child.
FBT recognizes that families often manage re-feeding and weight restoration for their loved ones, particularly when they are too young or developmentally compromised by their illness to assume responsibility themselves. In using FBT, we have developed an integrated program to engage families in the recovery process.
Nutritional Services
- We will work with your loved one to select a week’s worth of meals (options for breakfast, lunch, and dinner).
- We use an exchange system that is generally based on the American Diabetic Association standards.
- We do not focus on calories, which allows for flexibility and helps ensure that nutritional needs are met.
- Registered Dietitians support and answer any questions or concerns.
Depending on individual needs, we consider three meals and one to three snacks per day to be the norm. During meals, patients will be able to chat with peers and participate in light table games. Staff members will also join to help provide meal structure and support.
Food will initially be plated based on the menus that your loved one has selected (in accordance with the dietitian’s recommendations). As your loved one progresses in recovery, they will have the opportunity to incorporate buffet-style dining during mealtimes to practice portioning. As treatment progresses, they may also participate in restaurant outings and cooking groups.
Accommodating Special Dietary Requests
Eating Recovery Center takes food allergies seriously. Documentation of scientifically-proven food allergy testing is requested to accommodate your loved one’s needs, and we may also recommend further food allergy testing during treatment. When your loved one first meets with their dietitian, the staff will assess any special dietary requests (vegetarian, gluten-free, etc.) on a case-by-case basis. We may make accommodations for religious dietary practices, such as providing kosher meals for Jewish individuals.
We firmly believe that there are no ‘good’ or ‘bad’ foods; rather, we want your loved one to be exposed to a variety of foods. Our goal is to assess your loved one’s needs from a nutritional standpoint, and review each meal plan on an individual basis to help promote recovery. Throughout treatment, we encourage the understanding that all foods are acceptable in moderation.
Support for Adult Patients
While in treatment, adults receive medical and nutritional support from experienced professionals: all of whom address complications associated with a number of different eating disorders and mood, anxiety, and trauma-related conditions.
Therapeutic interventions like Acceptance and Commitment Therapy (ACT) are used to help adult patients learn how to create a rich, meaningful life in recovery. In using ACT, patients are supported and encouraged to identify what they value. Patients learn, internalize, and practice the tools to help them take committed action.
As adult patients move along the path of recovery, they can step down within the levels of care in our comprehensive service offerings. Stepping down to levels of care with more independence and autonomy helps patients protect their recovery as they reconnect with their lives outside of the treatment center – and allows them to test their skills while still operating within a structured, supportive environment.

Living Arrangements
At the Inpatient and Residential levels of care, patients live at the treatment center. At the Partial Hospitalization Program (PHP) level of care, patients attend an intensive day program – seven days a week – and live off-site at home or in nearby apartments.
As many patients do not live near their home, patients in PHP often choose to live in an ERC apartment setting. While apartments are not covered by insurance, arrangements can be made through Eating Recovery Center’s business office to purchase living space in low-cost apartment options.
Patients at the Intensive Outpatient Program (IOP) level live independently. Virtual IOP is additionally offered across the country for patients who require additional convenience and flexibility.


Family Support Services
As caregivers, you can actively help your loved one move through recovery. Regardless of whether you take an operative role in their treatment, or prefer a more hands-off approach, Eating Recovery Center offers an array of programming to support families, friends, and caregivers. These ongoing support services include:
- Hope Orientation
- Virtual Family & Friends Educational Series
- Family & Friends Educational Empowerment Webinar Series
- Caregiver Support Groups
- Family & Friends Resource Guide
- Family & Friends Activity Journal
For any questions regarding support and resources, reach out to the Community Outreach Liaison team at [email protected].
Nutritional Counseling for Eating Disorders
Nutrition plays a fundamental role in eating disorder treatment. Your loved one’s thoughts and behaviors around food are most likely negative and destructive, and many individuals need weight restoration in order to fully engage in therapeutic interventions. For those patients who are at a normal weight at the time of admission, nutrition exposure and education are critical in addressing underlying issues related to their relationship with food.
The nutrition philosophy at Eating Recovery Center emphasizes helping patients overcome their fear of food and eating by providing meal structure and support, education on a balanced pattern of nutrition, and collaborative care to achieve a healthy weight for optimal recovery.
Eating Recovery Center’s team of highly skilled Registered Dietitians work individually with patients at all levels of care to develop a personalized meal plan that works to achieve weight restoration and maintenance goals, and meet any verifiable dietary needs. Dietitians also work collaboratively with the entire multidisciplinary treatment team, and participate in meetings to support an integrated understanding of each patient’s progress and treatment goals.
In addition to individual nutrition counseling, Eating Recovery Center’s Registered Dietitians lead group education sessions. These staff members also oversee various exposure activities to deconstruct myths around food and offer opportunities to build confidence in food situations. Cooking classes, buffet-style meals, grocery shopping, and restaurant outings are integrated into treatment plans. These supplementary activities enable patients to develop the necessary skills to prepare them for success in real-life situations outside of treatment.
Learn about ERC's nutrition program.

The nutrition philosophy at Eating Recovery Center communicates that there are no 'good' or 'bad' foods - instead emphasizing balance, moderation, and variety.
Support for Children & Adolescent Patients
While in treatment, your loved one will receive medical and nutritional support from experienced professionals: all of whom address complications associated with a number of different eating disorders and mood, anxiety, and trauma-related conditions.
For patients ages 8 through 17*, our treatment approach is rooted in Family-Based Treatment (FBT) and Emotion-Focused Family Therapy (EFFT). FBT recognizes that families often manage re-feeding and weight restoration for their young loved ones when they are too developmentally young and/or compromised by their illness to assume responsibility for these tasks themselves. EFFT empowers parents to become agents of change in the recovery of their child.
Additional therapeutic interventions like Acceptance and Commitment Therapy (ACT) are used to help child & adolescent patients learn how to create a rich, meaningful life in recovery. In using ACT, patients are supported and encouraged to identify what they value. Patients learn, internalize, and practice the tools to help them take committed action. Treatment teams also draw from Dialectical Behavioral Therapy (DBT), Cognitive Behavioral Therapy (CBT), and Radically Open Dialectical Behavioral Therapy (RO-DBT).
As child & adolescent patients move along the path of recovery, they can step down within the levels of care in our comprehensive service offerings. Stepping down to levels of care with more independence and autonomy helps patients protect their recovery as they reconnect with their lives outside of the treatment center – and allows them to test their skills while still operating within a structured, supportive environment.
*Programming for ages 10 and under varies by treatment program and location.
Living Arrangements
At the Inpatient and Residential levels of care, patients live at the treatment center. At the Partial Hospitalization Program (PHP) level of care, patients attend an intensive day program – seven days a week – and live off-site at home.
Our child & adolescent patients can choose to live in a Ronald McDonald House, an Airbnb with family or friends, or an extended stay hotel. We will discuss the best living arrangements for your loved one and offer suggestions.
Patients at the Intensive Outpatient Program (IOP) level live independently with their families or caregivers. Virtual IOP is additionally offered across the country for patients who require additional convenience and flexibility.

Family Support Services
As caregivers, you can actively help your loved one move through recovery. Regardless of whether you take an operative role in their treatment, or prefer a more hands-off approach, Eating Recovery Center offers an array of programming to support families, friends, and caregivers. These ongoing support services include:
- Hope Orientation
- Virtual Family & Friends Educational Series
- Family & Friends Educational Empowerment Webinar Series
- Caregiver Support Groups
- Family & Friends Resource Guide
- Family & Friends Activity Journal
For any questions regarding support and resources, reach out to the Community Outreach Liaison team at [email protected].
Family Involvement for Child & Adolescent Patients
A hallmark component of our treatment approach for children and adolescents is our innovative family programming: parents are empowered to become agents of change for their young ones, as well as support persons to help them sustain future, long-term recovery.
Your child may require Inpatient and/or Residential care, or they may enter treatment at the Partial Hospitalization Program (PHP) level. When your loved one is in PHP, you will participate in practical, hands-on activities – including meal-time planning – to prepare you and your child for life back home.
Over time, your child will spend less time in PHP and more time with you in “real-life” situations before returning home. Family meals, outings, and passes are available as your child moves forward in treatment and recovery.
In addition to opportunities designed to help your child acclimate back into “real-life,” we will ask you to help create your child’s “aftercare plan.” This process involves thinking through and making plans to address the challenges of recovery in the home environment.


Nutritional Support Services
Nutrition plays a fundamental role in treatment: nourishing your child’s body is an important first step.
- If weight restoration is needed, our medical and nutritional staff will carefully and safely manage refeeding.
- For patients at a healthy weight, nutrition exposure and education will help address underlying issues related to their relationship with food.
- A highly skilled Registered Dietitian will work with your child to support them in overcoming fears around food and eating.
- Dietitians work collaboratively with the treatment team to support an integrated understanding of each patient’s progress and treatment goals.
- In addition to individual nutrition counseling, Dietitians lead group educational sessions and oversee various exposure activities to build confidence in real-life food situations.
- Our expert staff of clinicians regularly dine with patients to provide structure and create a therapeutic, supportive meal environment.
- Staff supervision at meals provides the encouragement, redirection of eating disordered behaviors, and role modeling necessary to affect behavior change.
- Dietitians work closely with parents and caregivers to teach the skills and fundamentals of nutrition, food portioning, and food plating: helping you continue meal planning and meal support for your child after treatment.
Learn about ERC's nutrition program.
School During Treatment
Missing school can be a source of anxiety, especially when a student is absent from class because they are in treatment. At Eating Recovery Center, patients and their families do not have to choose between staying in school or getting treatment for eating disorders.
We understand the importance of continuing education while in treatment, and work with our patients to prepare them for academic success after treatment.
- Education Specialists support patients with their daily schoolwork – helping ensure a sense of normalcy – and support them as they transition back to school
- Education Specialists serve as your child’s advocates: helping them understand there is a plan for continued education, and allowing them to feel comfortable putting recovery first
- Education Specialists ensure any material that schools send is taught in an appropriate way: promoting mental wellness by lessening the anxiety of missed assignments All therapists work with patients to continue to develop the skills needed to function well at school
At time of discharge, education transition plans and recommendations are sent to your child’s school to support the transition back into an academic environment. If your child admits during summer vacation, independent learning projects and book clubs are incorporated into treatment plans.
Learn about ERC's education specialists.


Hide Last Child Layout Div
styles
menu