Clinically reviewed by
Adee Levinstein, MS, RD, LD, CEDS-C
Suggestions
Common Searches
Eating disorders aren’t just about food — and you can’t recover from an eating disorder without food. In eating disorder treatment, food is your medicine. Without it, your brain and body cannot heal from the damage the eating disorder has caused.
No matter what your symptoms look like, you deserve to have a peaceful relationship with food and your body. In treatment, you will learn how to align your actions with your values, reprioritizing food as one of the many important parts of your life. Over time, as your brain and body heal, you become less preoccupied with food and/or weight.
On this page, we walk you through nutritional therapy and psychoeducation provided at Eating Recovery Center. We also answer frequently asked questions related to nutrition and meal support.
Eating Recovery Center recognizes the inherent diversity in human bodies and welcomes people of all body shapes and sizes to our weight-inclusive treatment centers. As we focus on health-promoting behaviors, our goal is to take care of you — a whole person — and to help you make choices that support a full, values-aligned life.
Weight-inclusive care means better care for folks in diverse bodies — and it counters weight stigma, a form of discrimination based on a person’s weight or size.
"No matter what your symptoms look like, you deserve support in fostering a peaceful relationship with your body, food and movement. There is hope for a full and lasting recovery – your life can be different."

Meals play a crucial role in eating disorder treatment and are a critical step towards nutritional rehabilitation. In treatment, patients plan meals with their registered dietitians weekly, reviewing and adjusting meals, food preferences and goals, as needed.
Mealtime can be difficult, and you will feel challenged. By approaching food in a more balanced way, you can move towards a full and lasting recovery. Through collaborative meal planning with your treatment team, normalized eating patterns can return.
For those in on-site care in our inpatient and residential programs, you will typically have three meals and three snacks daily with peers. As you progress through treatment, you will start to have meals and snacks off the unit, with family members and during outings. Some sites offer cooking group experiences as well as grocery store tours.
Nutritional rehabilitation is the process of healing malnutrition caused by an eating disorder. This process helps you return to an optimal nutritional status by:
If you’ve been restricting your food intake, you could be experiencing symptoms of malnutrition. Malnutrition can affect people of all body weights, shapes and sizes, harming the brain and body.
Nutritional rehabilitation works by resolving most, if not all, of the physical and mental health consequences the eating disorder has caused. There are many benefits to nutritional rehabilitation, including:
Nutritional rehabilitation is overseen by experienced psychiatrists, registered dietitians, therapists, primary care physicians and nurses who collaborate daily on-site to provide you with the highest quality nutritional care.
"Food is our patients’ number one medication. Without appropriate nutrition, patients’ brains and bodies cannot heal from the devastation of the eating disorder. When food intake does not meet their body’s needs, they won’t get better. Adequate nutrition is vital to recovery; we provide that here."
Patients receive support in planning their meals for the week, including breakfast, lunch, dinner and snacks. Adults choose their own menus and caregivers plan menus for child and adolescent patients. The treatment team monitors and evaluates each patient’s nutritional status, adjusting meal plans as needed. Exchange-based meal plans offer flexibility, ensuring that nutritional needs are met.
When you arrive for treatment, please discuss any food allergies or dietary needs with your registered dietitian.
Adult patients are encouraged to use the Recovery Record app in treatment and after discharge. Parents log in and update the app for child and adolescent patients. This app offers many convenient benefits to those in eating disorder recovery and is widely praised throughout the field. With help from the app, you will be able to:
The Recovery Record app is available for free in your favorite app store.

Mealtime in eating disorder treatment can be challenging and anxiety-provoking. Individuals may feel discomfort due to the refeeding process, challenging their eating disorder rules or for other reasons. During mealtimes and snacks, the treatment team works closely with each patient to provide structure and emotional support. Eating disorder behaviors are monitored and addressed. All of our meal rooms are designed to be as pleasant and welcoming as possible.
Many people seeking eating disorder treatment have complicated relationships with food. As you move through treatment, you will learn new coping skills to help you manage anxiety and other difficult emotions that come up around food. During meals, the treatment team addresses eating disorder thoughts and behaviors using a variety of approaches:
People with eating disorders, including those with avoidant/restrictive food intake disorder (ARFID), can be fearful of eating certain foods or entire food groups. We call these foods “fear foods.” Prior to coming to treatment, patients often consider these foods off-limits. In treatment, we work to re-integrate these foods back into one’s meals. Staff work closely with patients as they start to eat “fear foods” again. This is highly individualized and looks different for each person and each diagnosis.
"At Eating Recovery Center, families are an essential and active part of their child’s treatment plan. When an individual has an eating disorder, they are often unable to make healthy choices for themselves. We incorporate family-based treatment into our program to help caregivers learn how to manage meals — eventually eliminating eating disordered behaviors. Our therapists serve as coaches, guiding families through the process."

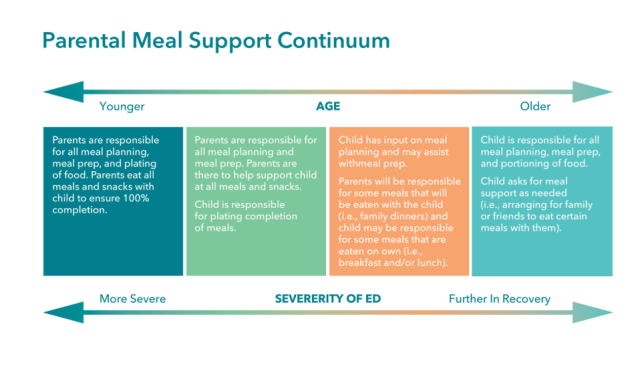
Through our innovative family program, caregivers are empowered to become agents of change for their loved ones, helping them achieve long-term recovery. Our family-based treatment model views caregivers as an essential part of the treatment plan for child and adolescent patients. Caregivers manage certain aspects of each young patient’s meals. The goal is to eventually eliminate eating disorder behaviors.
The following principles serve as a foundation for our behavioral approach to treatment:
Our therapists also serve as coaches, guiding families through the treatment process. Caregivers learn how to support their children through behavior coaching and emotion coaching. These strategies can help caregivers strengthen their relationships with their loved ones as they recover from the eating disorder.
We expect a primary caregiver to be involved in treatment with all of our child and adolescent patients. It is essential that at least one caregiver learn the necessary skills to support the patient’s long-term recovery, including preparing a successful home environment. In treatment, we work together to:

Nutritional counseling and education groups are a fundamental part of eating disorder treatment. During these sessions, you will receive professional and peer support and nutrition education on a variety of topics, along with:
Families and caregivers are also encouraged to attend nutrition education and support groups designed to teach them how to support their loved ones.
Patients come to us with a variety of backgrounds, behaviors and beliefs. Our goal is to provide nutritional rehabilitation that safely helps them achieve optimal physical and mental health. At times, patients need an extra layer of support.
Most patients with eating disorders experience co-occurring mental health concerns, therefore:
Additionally, our on-site programs are staffed with medical doctors and nurses who continuously monitor patients to reduce the risk of physical health complications. Registered dietitians are medically trained to work with patients dealing with physical health concerns, including:
Our hope is that patients are able to complete the meals and snacks included in their treatment plan. However, we understand this can be challenging. We provide supplements and tube feeding as a “Plan B” for those who are unable to finish meals and snacks. First, we offer a number of incentives to our patients to help them complete meals and snacks. Then, we refer to established guidelines before making a recommendation for supplements or tube feeding.
At times, patients struggle to complete their meal plans and need a little more support as part of their nutritional rehabilitation. Supplements help patients meet their nutritional needs so their brains and bodies can heal.
In some instances, patients are unable to complete their meal plans and supplements. When this occurs, tube feeding may be recommended. This procedure can be vital and lifesaving. When tube feeding is recommended, our experienced medical and nursing staff provide temporary nutritional supplementation via tubes inserted through the nose.
We are one of the few eating disorder treatment programs who are able to offer tube feeding on-site in our residential programs. The benefit of this service is that patients can stay with their residential treatment team instead of leaving to go to a separate hospital or location, which can be upsetting and disruptive to treatment.
Refeeding syndrome is a potentially fatal complication that can occur when patients start to eat after a long period of restriction. Our medical doctors and nurses monitor all patients to reduce the risk of refeeding syndrome with established guidelines that include:

Our binge eating disorder treatment program is based on a weight-inclusive approach that incorporates:
These interventions can bring positive outcomes to all patients, including:

Coming soon...
Hide Last Child Layout Div
© 2025 Eating Recovery Center. All rights reserved. Terms & Conditions | Privacy Policy